Introduction: In the study of mental health, it is essential to differentiate between various classifications of disorders, each characterized by specific symptom profiles, etiologies, and therapeutic approaches. Two primary categories—mood disorders and personality disorders—represent distinct forms of mental health conditions that, while occasionally presenting overlapping symptoms, have unique impacts on an individual’s functioning and quality of life. Mood disorders, which include conditions such as major depressive disorder and bipolar disorder, are primarily characterized by persistent alterations in affective states. These disorders involve episodic shifts in mood that often occur independently of external factors and can exhibit cyclical patterns of remission and recurrence. Conversely, personality disorders are defined by enduring and pervasive patterns of behavior, cognition, and emotional experience that are rigid, maladaptive, and deeply embedded in an individual’s personality structure. Examples include borderline personality disorder (BPD) and narcissistic personality disorder (NPD), both of which affect interpersonal interactions, self-concept, and relationship dynamics in a more stable and pervasive manner than mood disorders. (19)
This analysis seeks to elucidate the fundamental distinctions between mood disorders and personality disorders, examining their respective diagnostic criteria, symptomatology, and therapeutic challenges. By addressing these differences, this discussion aims to foster a deeper understanding of these mental health conditions, promote destigmatization, and underscore the importance of accurate diagnosis and individualized treatment strategies in the field of mental health care.
Table of Contents
Mood disorder definition

Mood is characterized as an enduring, pervasive internal emotional state that significantly influences an individual’s behavior across various domains of external interactions. Mood disorders encompass conditions marked by substantial emotional dysregulation, manifesting as extreme low moods (depression) or elevated moods (hypomania or mania). Key disorders within this category include bipolar disorder, cyclothymia, hypomania, major depressive disorder, disruptive mood dysregulation disorder, persistent depressive disorder, and premenstrual dysphoric disorder. These mood disorders are prevalent psychiatric conditions associated with increased rates of morbidity and mortality. (1),(19)
Types of mood disorders
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), classifies mood disorders into two primary categories: bipolar disorders and depressive disorders. Bipolar disorders are further subdivided into bipolar I, bipolar II, cyclothymic disorder, bipolar disorder associated with another medical condition, substance/medication-induced bipolar disorder, other specified bipolar disorders, and unspecified bipolar disorders. list of mood disorders: (20)
- Bipolar I disorder is characterized by the presence of a full manic episode, which includes an elevated mood accompanied by at least three of the following symptoms: increased goal-directed activity, grandiosity, reduced need for sleep, distractibility, racing thoughts, pressured speech, and impulsive behavior. These symptoms must persist for at least one week or require hospitalization. If the mood is irritable rather than elevated, at least four symptoms must be present to meet the criteria for a manic episode.
- Bipolar II disorder involves a history of major depressive episodes combined with periods of hypomania, each lasting at least four days.
- Cyclothymic disorder is defined by a long-standing pattern of subthreshold mood disturbances, including mild hypomanic and depressive episodes, without meeting the full criteria for mania, hypomania, or major depression. This disorder is diagnosed in adults who experience at least two years of fluctuating hypomanic and depressive episodes, while children and adolescents must experience these symptoms for a minimum of one year to be diagnosed with cyclothymia.
- Hypomania is a milder, non-psychotic form of mania that lasts for at least four consecutive days, with symptoms such as elevated or irritable mood and at least three (or four in the case of irritability) of the following: increased goal-directed activity, grandiosity, reduced sleep, distractibility, racing thoughts, pressured speech, and risky behaviors. According to the International Classification of Diseases 11th Revision (ICD-11), both cyclothymia and hypomania are considered precursor states to bipolar disorders. Furthermore, in the DSM-5, hypomania is a core feature of bipolar II disorder. (21)
Imagery-based techniques utilize mental imagery to promote cognitive and emotional changes. These methods offer a dynamic approach to examining and altering an individual’s internal experiences. Imagery-based cognitive therapy for bipolar disorder and mood instability has shown promise in treating by utilizing mental imagery techniques to address maladaptive thought patterns and emotional regulation. (2)
Neuropsychiatry is integral to the diagnosis, management, and understanding of mood disorders, including depression, bipolar disorder, and anxiety-related conditions. What is Neuropsychiatry? It merges concepts from both neurology and psychiatry to explore and address the complex interactions between brain activity, emotional regulation, and behavioral outcomes. This multidisciplinary approach provides insights into the pathophysiology of mood disorders and facilitates the development of effective treatment strategies. (3),(22)
Mood disorder symptoms

The manifestation of mood disorders varies depending on age and the specific type of mood disorder, with individuals experiencing different symptoms when affected by depression. Common symptoms associated with mood disorders include persistent feelings of sadness, anxiety, or emptiness, along with a sense of hopelessness or helplessness. Individuals may also exhibit low self-esteem, feelings of inadequacy or worthlessness, and excessive guilt. A lack of interest in previously enjoyable activities, including sexual activity, is often observed, as are interpersonal difficulties.
Other symptoms may include disturbances in sleep patterns (either insomnia or hypersomnia), changes in appetite or weight, decreased energy levels, and impaired concentration. Decision-making abilities may be compromised, and frequent unexplained physical complaints such as headaches, stomachaches, or chronic fatigue may persist despite medical treatment.
Cognitive and mood disorders are often interrelated, with disruptions in brain function and neurochemistry contributing to impairments in both mental processing and emotional regulation. Depression may lead to cognitive changes, including deficits in executive function, impairments in learning and memory, diminished attention and concentration, and decreased processing speed. Various treatment options are available to address these cognitive effects. (4),(23)
Neuropsychiatric symptoms frequently co-occur with dementia, manifesting as agitation, depression, apathy, delusions, hallucinations, and disruptions in sleep. In certain cases, these symptoms cluster into identifiable syndromes, which has led to the development of operational criteria for specific psychotic or mood disturbances associated with dementia.
In some cases, individuals may express suicidal ideation, engage in threats of self-harm, or show heightened sensitivity to failure or rejection. Increased irritability, hostility, or aggression may also occur. The intensity and duration of these symptoms typically exceed those experienced by individuals without mood disorders, and they can significantly disrupt social, familial, or professional functioning. (22)
Given the potential severity of symptoms, especially the presence of suicidal thoughts, immediate medical intervention is essential. If access to a primary care provider is delayed, individuals should seek care from a qualified mental health facility. Since the symptoms of mood disorders can resemble other mental health conditions, a thorough evaluation by a healthcare provider is necessary for accurate diagnosis and appropriate treatment. (5)
What are mood disorders related to?
Environmental factors such as significant life stressors—including the loss of a loved one, chronic stress, traumatic experiences, and early-life abuse—are strongly associated with an increased risk of developing mood disorders, particularly depression, later in life. Although the precise mechanisms behind mood disorders remain unclear, they are believed to arise from a complex interplay of factors, including neurobiological changes, imbalances in brain chemistry, genetic predispositions, certain medical conditions, and exposure to psychoactive substances.
While temporary sadness is a normal response to challenging circumstances, mood disorders are characterized by more intense and enduring symptoms that are notably harder to control. Individuals of all ages who have a parent with a mood disorder are at an elevated risk of experiencing similar conditions. (5),(25)
Is mood disorder a disability?
Patients with mood disturbances often experience significant difficulty in daily functioning. Common diagnoses include dysthymic disorder, major depression, and bipolar disorder. In more severe instances, the fluctuations in mood can become overwhelming, rendering daily tasks nearly impossible. While many individuals filing for disability benefits are impacted by physical illnesses, others are affected by mental health conditions. Affective disorders, or mood disorders, are among the mental health conditions that may qualify an individual for disability benefits, depending on the specific circumstances. (4), (25)
here are more information about mood disorders:
What is true about mood disorders?
Mood disorders significantly impact individuals’ quality of life. During depressive episodes, individuals may experience symptoms such as irritability, feelings of worthlessness, and a loss of interest in previously valued activities. Suicidal thoughts or behaviors can also occur. For a clinical diagnosis of a mood disorder, these symptoms must persist for several weeks or more. Mood disorders can lead to behavioral changes and impair one’s ability to carry out everyday tasks, including responsibilities at work or school. Major depressive disorder and bipolar disorder are among the most prevalent mood disorders.
Which of the following statements is true of mood disorders?
- The level of social and occupational functioning of bipolar I and bipolar II disorders are identical.
- Hypomania is a diagnostic criterion for bipolar II disorder but not for cyclothymic disorder.
- A diagnosis of cyclothymic disorder requires that the person alternates between cycles of hypomanic symptoms and depressive symptoms.
- A major depressive episode is necessary for a diagnosis of bipolar I disorder.
Explanation:
Cyclothymic disorder is characterized by alternating periods of hypomanic and depressive symptoms that do not meet the diagnostic criteria for a full hypomanic episode or a major depressive episode. Bipolar I and Bipolar II disorders are distinguished by differences in the severity of mood episodes, and the degree of social and occupational functioning can vary significantly among individuals, making it inappropriate to assume their functional levels are identical. Hypomania is a critical diagnostic feature of Bipolar II disorder, although it is not exclusive to this condition, as it is also included in the diagnostic criteria for cyclothymic disorder. In contrast, a major depressive episode is not a requisite for Bipolar I disorder; the essential criterion for this diagnosis is the occurrence of at least one manic episode, with the presence of a depressive episode being optional. (7)
Which statement about mood disorders and digital technology is true?
- Connecting with others digitally makes mood disorders worse.
- Overuse of technology causes mood disorders, including anxiety and depression.
- Connecting with friends on social media platforms is the best way to relieve mood disorders.
- If you’re likely to develop a mood disorder, overusing digital technology might make it worse.
Explanation:
Studies indicate that prolonged engagement with digital technologies, including social media and excessive screen time, may have adverse effects on mental health, particularly in individuals with a preexisting susceptibility to mood disorders such as anxiety or depression. This overuse has been linked to increased feelings of isolation, stress, and negative emotional states. However, it is important to note that digital technology use is not the sole determinant in the onset or exacerbation of mood disorders.
Connecting with others digitally makes mood disorders worse by increasing feelings of isolation, reducing face-to-face interactions, and potentially exposing individuals to negative social comparisons. Excessive use of digital technology appears to heighten the risk of mood disorders, particularly in individuals with a predisposition to such conditions. However, the impact varies based on individual circumstances. Research indicates a correlation between extensive digital engagement and heightened symptoms of depression and anxiety. Specifically, prolonged social media use is associated with increased feelings of anxiety, isolation, and depression. This may stem from users comparing themselves to idealized portrayals of others’ lives, which can lead to feelings of inadequacy and dissatisfaction.
It is important to consider that individuals respond to digital technology in diverse ways. While some may benefit from moderate use of social media or other digital platforms for social support and maintaining connections, others may find it detrimental. For instance, connecting with friends on social media platforms has been suggested as a beneficial method for relieving symptoms of mood disorders by fostering social support and enhancing emotional well-being. The effects depend on individual predisposition, personal circumstances, and patterns of technology use. (9)
Do you know Which of the following is the most common mood disorder related to digital technology?
- Anxiety
- Depression
- Bipolar disorder
- Schizophrenia
Digital technology, particularly social media, is increasingly linked to mood disorders, with anxiety—specifically social anxiety and generalized anxiety—being among the most common. This association is largely attributed to continuous online connectivity, frequent notifications, and the social comparison pressures that social media platforms often encourage. Excessive engagement with digital media can exacerbate mood disturbances, including both anxiety and depression, by disrupting sleep, hindering in-person social interactions, and potentially altering neural functioning. Social media has been shown to detrimentally impact psychological well-being by contributing to anxiety, depressive symptoms, feelings of loneliness, and the phenomenon known as “fear of missing out” (FOMO). These effects are notably pronounced in adolescent and young adult populations. Given its pervasive and evolving nature, social media is likely to become even more embedded in daily life, with possible further implications for mental health. If you’re likely to develop a mood disorder, overusing digital technology might exacerbate the condition by disrupting sleep patterns and increasing stress levels. (8)
Key factors influencing mood disorders in relation to digital technology include:
- Social Comparison: Interaction with highly curated online profiles frequently prompts social comparison, which can foster feelings of inadequacy and reduced self-esteem, correlating with elevated anxiety and depressive symptoms.
- Notification Overload: Persistent exposure to notifications and the expectation to remain constantly connected can lead to increased stress levels and feelings of overwhelm.
- Sleep Disturbance: The use of digital devices before bedtime disrupts natural circadian rhythms, negatively impacting sleep quality and, subsequently, mood stability.
- Cyberbullying: Exposure to online harassment is a notable risk factor for anxiety and depression, especially in adolescents and young adults.
Personality disorders

Personality disorders are a category of psychiatric conditions marked by persistent maladaptive patterns of behavior, cognition, and emotional experience that are exhibited across various contexts and diverge from cultural norms. These disorders involve enduring tendencies in individuals to perceive themselves and interact with others in ways that lead to significant interpersonal difficulties. Individuals with personality disorders frequently experience challenges in emotional regulation, distress tolerance, and impulse control. These dysfunctions contribute to interpersonal difficulties and may negatively impact familial relationships, social interactions, occupational and academic performance, and overall life satisfaction.
If you experience symptoms indicative of a personality disorder, it is advisable to consult a healthcare provider or mental health specialist. Untreated personality disorders can lead to significant impairments in interpersonal relationships and emotional regulation. Additionally, the capacity to perform daily activities and achieve personal objectives may decline in the absence of appropriate intervention. (11)
Personality disorders vs mood disorders
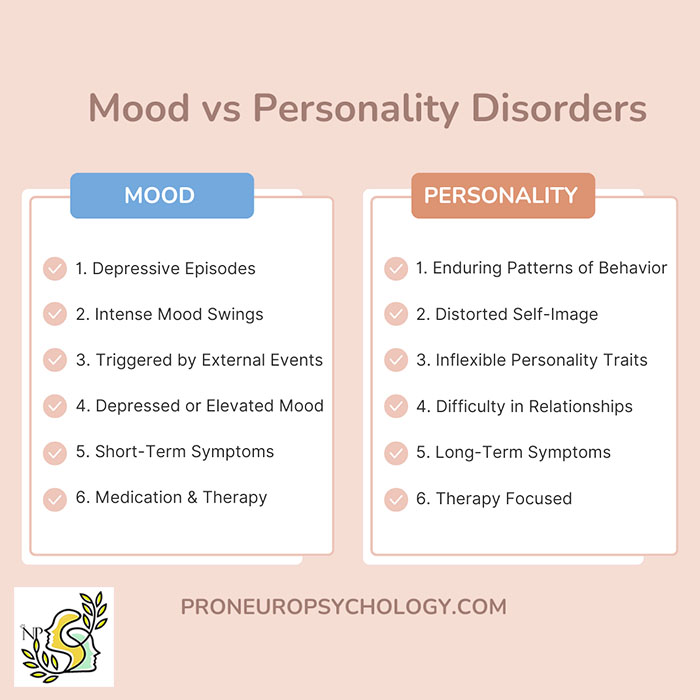
The term “mental health condition” encompasses a wide range of disorders that impact an individual’s psychological well-being, including both mood and personality disorders, which are distinct classifications of mental illness. Mood disorders are characterized by episodic disturbances in mood, such as depressive or manic episodes, which may vary in intensity and duration over time. In contrast, personality disorders involve persistent patterns of behavior and internal experiences that remain stable across different situations and over extended periods. Despite their differences, mood and personality disorders can present with overlapping symptoms, which may complicate both diagnosis and public understanding.
Adjustment disorder with/ depressed mood
An adjustment disorder represents an intense psychological response to a significant stressor, which may be either a positive or negative life event. This disorder manifests as short-term emotional, cognitive, and behavioral disturbances that are disproportionate to the typical response expected to the stressor. Various subtypes of adjustment disorder exist, and treatment typically involves psychotherapy, with medication being used in some cases.
Adjustment disorder with depressed mood is characterized by emotional symptoms such as persistent sadness, feelings of hopelessness, frequent crying, and anhedonia, or the inability to derive pleasure from previously enjoyable activities. Adjustment disorder with anxiety involves symptoms of excessive worry, anxiety, and a sense of being overwhelmed, often accompanied by difficulties in concentration. In children, separation anxiety is frequently a prominent symptom.
Conclusion
In summary, mood disorders and personality disorders represent distinct classifications of mental health conditions, each defined by specific features. Mood disorders, including depression and bipolar disorder, are primarily characterized by fluctuations in emotional states, which may be triggered by internal or external stressors, and typically present as episodic mood disturbances that are transient in nature. Conversely, personality disorders, such as borderline or antisocial personality disorder, are marked by pervasive and enduring patterns of behavior, cognition, and interpersonal interactions that diverge significantly from societal norms and remain stable over time. Although both disorders may share overlapping symptoms, such as emotional instability, the fundamental distinction lies in the temporality of the symptoms, with mood disorders focusing on short-term emotional changes and personality disorders on consistent, long-term behavioral and emotional patterns.

Frequently Asked Questions
Frequently Asked Questions about mood disorders:
What are the two key moods involved in mood disorders?
The two key moods involved in mood disorders are depression (lows) and mania/hypomania (highs).
Is mood disorder normal?
No, mood disorders are not normal, but it’s normal to experience some mood swings.
What do most researchers believe that mood disorders are caused by?
Stressful life changes (death of significant other, parents, siblings, etc.) traumatic events and childhood abuse have been found to be major risk factors for the development of mood.
References:
- https://pubmed.ncbi.nlm.nih.gov/34881733/
- https://pubmed.ncbi.nlm.nih.gov/29851879/
- https://pubmed.ncbi.nlm.nih.gov/39088414/
- https://pubmed.ncbi.nlm.nih.gov/25701910/
- https://pubmed.ncbi.nlm.nih.gov/36004528/
- https://pubmed.ncbi.nlm.nih.gov/35139458/
- https://pubmed.ncbi.nlm.nih.gov/29933949/
- https://pubmed.ncbi.nlm.nih.gov/29368960/
- https://pubmed.ncbi.nlm.nih.gov/24524714/
- https://pubmed.ncbi.nlm.nih.gov/31705498/
- https://pubmed.ncbi.nlm.nih.gov/37858331/
- https://pubmed.ncbi.nlm.nih.gov/37661007/
- https://pubmed.ncbi.nlm.nih.gov/38694944/
- https://pubmed.ncbi.nlm.nih.gov/39084841/
- https://pubmed.ncbi.nlm.nih.gov/38302210/
- https://pubmed.ncbi.nlm.nih.gov/38614452/
- https://pubmed.ncbi.nlm.nih.gov/38341336/
- https://pubmed.ncbi.nlm.nih.gov/38176542/
- https://link.springer.com/article/10.1007/s11920-006-0051-x
- https://www.sciencedirect.com/science/article/abs/pii/S1877341909700376
- https://www.sciencedirect.com/science/article/abs/pii/S1476179306700350
- https://journals.lww.com/co-neurology/citation/1988/01040/neuropsychiatry.8.aspx
- https://www.psych.theclinics.com/article/S0193-953X(03)00106-0/abstract
- https://psycnet.apa.org/record/2009-07509-022
- https://www.mdpi.com/2227-9059/12/3/574



