Introduction: Clinical neuropsychology is a specialized branch of psychology that examines the relationship between brain function and behavior, particularly in the context of neurological disorders and injuries. This field combines insights from both psychology and neurology to understand how the structure and function of the brain influence cognitive abilities, emotions, and behavior. Neuropsychologists use this knowledge to assess, diagnose, and treat individuals with various conditions, such as traumatic brain injuries, strokes, dementia, and developmental disorders. The origins of clinical neuropsychology date back to the 19th century when researchers began exploring the links between brain lesions and cognitive deficits. Early pioneers like Paul Broca and Carl Wernicke established foundational concepts by identifying specific brain regions responsible for speech and language processing. This essay aims to provide a comprehensive overview of clinical neuropsychology, highlighting its contributions to our understanding of the brain-behavior relationship and its vital role in treating neurological conditions.
Table of Contents
Clinical neuropsychology
Clinical neuropsychology is an applied science concerned with the behavioral expression of brain dysfunctions. A neuropsychological examination may have four different objectives: diagnosis, patient care, treatment, and research.
Clinical neuropsychology definition
what is clinical neuropsychology? Clinical Neuropsychology is a specialty field within clinical psychology, dedicated to understanding the relationships between brain and behavior, particularly as these relationships can be applied to the diagnosis of brain disorder, assessment of cognitive and behavioral functioning and the design of effective treatment. Neuropsychology draws information and material from neurology, cognitive psychology, and psychiatry and also act as a junction point for investigators belonging to related disciplines. Its central aim is to understand how brain functioning influences behavior and cognition. Clinical Neuropsychologists complete comprehensive assessments of cognition, emotion and behaviour and prepare reports for clients and health professionals.
Clinical Neuropsychologist
Clinical neuropsychology is a scientific discipline focused on understanding and applying the relationships between brain function and behavior. A Clinical Neuropsychology PhD program provides advanced training in understanding brain-behavior relationships, preparing students for careers in both research and clinical practice.
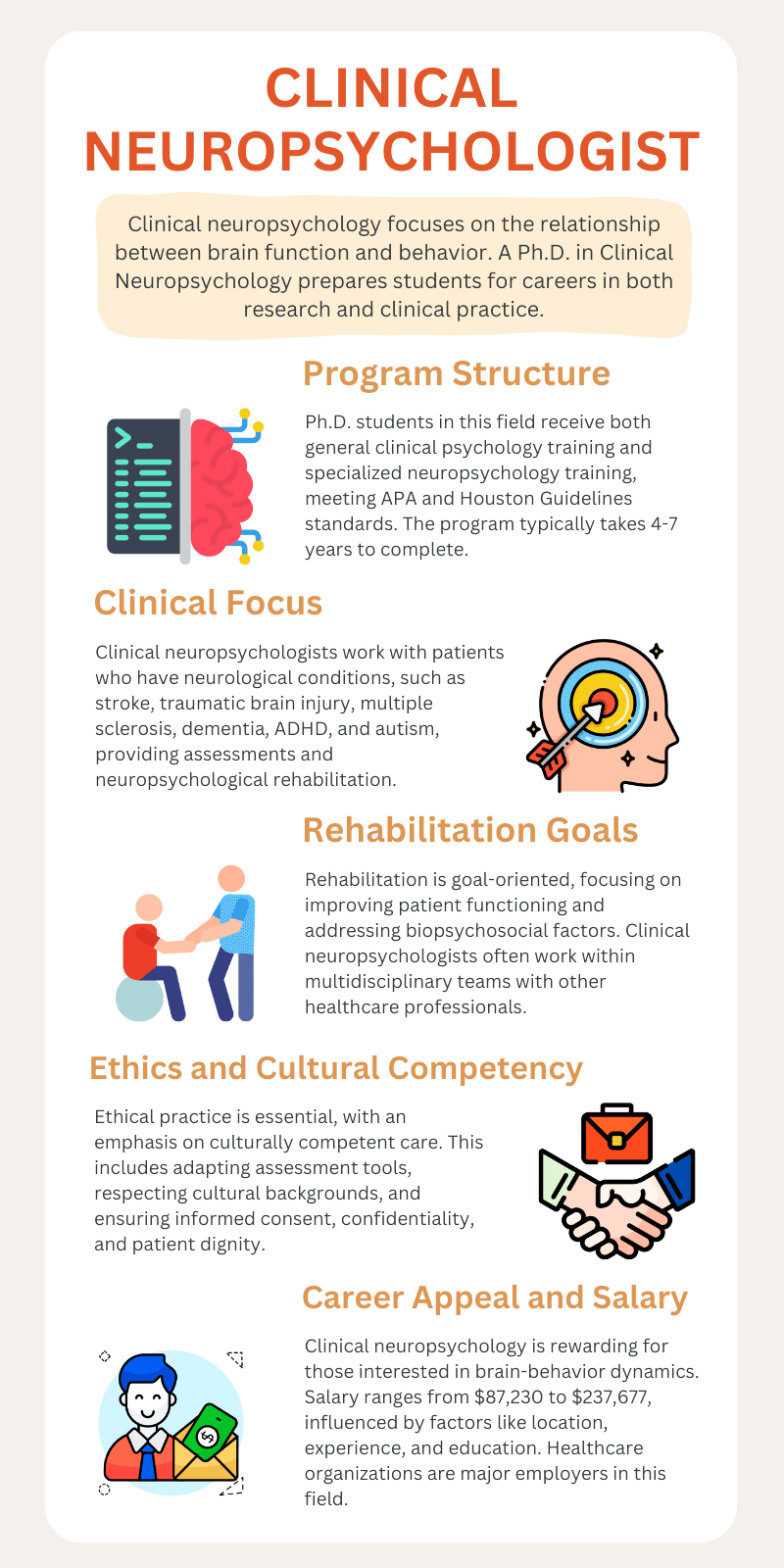
Ph.D. students specializing in Clinical Neuropsychology receive comprehensive training in general clinical psychology, as well as specialized training in neuropsychology. This training aligns with the American Psychological Association (APA) requirements for doctoral education in clinical psychology and follows the Houston Guidelines for neuropsychology training. A doctoral degree is essential for pursuing a career in this field. Depending on their research interests, students typically take four to seven years to complete their programs.
Clinical neuropsychologists work with individuals who have, or are suspected to have, conditions affecting the brain or central nervous system. These conditions may include stroke, traumatic brain injury, multiple sclerosis, dementia, functional neurological symptoms, ADHD, and autism. They provide neuropsychological rehabilitation to those with brain injuries or neurological diseases, utilizing a range of psychological models. Rehabilitation efforts are generally goal-oriented, aiming to enhance functioning and address the biopsychosocial factors that influence the client. Clinical neuropsychologists often collaborate as part of multidisciplinary teams that include neurosurgeons, neurologists, and other healthcare professionals.
Ethically, neuropsychologists must be aware of potential biases that may affect their clinical judgment and strive to provide culturally competent care. This entails not only adapting assessment tools to be culturally relevant but also maintaining a strong commitment to informed consent, confidentiality, and the dignity of each client. Ultimately, prioritizing cultural and ethical considerations in neuropsychology enhances the effectiveness of treatment and fosters trust and collaboration between practitioners and clients. Cultural and ethical considerations in neuropsychology play a crucial role in ensuring that assessments and interventions are appropriate and respectful of diverse populations. These considerations involve understanding the unique cultural backgrounds, beliefs, and values of individuals, which can significantly influence their cognitive functioning and behavior.
If you are intrigued by how the brain functions and its impact on human behavior, a career in neuropsychology can be quite rewarding. Earning potential is also an important consideration for this profession The clinical neuropsychology salary varies depending on location, experience, and education level. The average salary for neuropsychologists ranges from approximately $87,230 to $237,677 per year Healthcare organizations are the primary employers of neuropsychologists.
Here you can listen to one of the most complete podcasts on how to become a neuropsychologist from Navigating Neuropsychology Podcast.
Difference between a neuropsychologist and a clinical neuropsychologist
There is difference between a neuropsychologist and a clinical neuropsychologist. A field of neuropsychology focuses on understanding how brain function influences cognitive processes and behavior.
Here you will find a brief and useful explanation from Dr. Fadi Tayim:
There are two main types of neuropsychologists.
Cognitive neuropsychologists: These experts conduct research that helps further the field of neuropsychology.
Clinical neuropsychologists: These experts work directly with people seeking care and other healthcare providers.
Psychologists who provide clinical or counseling services assess and treat mental, emotional and behavioral disorders. They use the science of psychology to treat complex human problems and promote change. They also promote resilience and help people discover their strengths. Clinical psychology focuses on diagnosing and treating mental health disorders through various therapeutic approaches.
Clinical neuropsychological assessment

Introduction to Clinical Neuropsychology offers a comprehensive understanding of the connection between brain function and behavior, emphasizing the assessment and treatment of cognitive and psychological disorders. A clinical neuropsychological evaluation is a vital tool for assessing mental and psychiatric functioning, particularly following a brain injury or illness.
Individuals who have experienced traumatic brain injuries, concussions, epilepsy, or neurodegenerative conditions such as Alzheimer’s disease or Parkinson’s disease are often referred for clinical neuropsychological assessments. These evaluations provide a detailed understanding of how an individual’s brain functions and play a crucial role in distinguishing between typical age-related cognitive changes and early signs of dementia in older adults. There are several specific uses of neuropsychological assessment, including:
- Collection of diagnostic information
- Differential diagnostic information
- Assessment of treatment response
- Prediction of functional potential and functional recovery
Common neuropsychological disorders include conditions such as Alzheimer’s disease, ADHD, and traumatic brain injury. Clinical Neuropsychology is concerned with the assessment and rehabilitation of people with brain injury, neurological disease or neurodevelopmental conditions. Clinical Neuropsychologists are specially trained to understand the relationship between brain and neuropsychological function.
The role of neuropsychologists in rehabilitation is essential for assessing and treating cognitive and emotional challenges following brain injuries, neurological conditions, Neurodegenerative diseases, Neurocognitive disorders, Brain-behavior relationships and Cognitive impairment.
Brain injury
Brain injury (BI) refers to the destruction or degeneration of brain cells, which can occur due to various internal and external factors. Generally, brain damage signifies significant trauma-induced harm that is often indiscriminate. Clinical neuropsychologists specialize in evaluating patients with brain injuries and create treatment plans based on a thorough assessment of their symptoms.
Brain injury (TBI), in particular, can greatly affect working memory, mental flexibility, long-term memory, and attention span. Clinical neuropsychological assessments are essential in identifying which areas of the brain have been affected by a BI and how these impairments influence daily functioning. Additionally, testing can reveal how other factors, such as depression, anxiety, and life stress, might be impacting cognitive performance. Neuropsychological interventions can help individuals recover cognitive functions after brain injuries.
Traumatic brain injury (TBI)
Traumatic brain injury (TBI) typically occurs as a result of a violent blow or jolt to the head or body. It can range from mild with temporary dysfunction to severe with long-term complications or even death. An object that penetrates the skull and goes through brain tissue, such as a bullet or a shattered piece of bone, can also cause traumatic brain injury. The damage to the brain can lead to a wide array of cognitive, emotional, and physical symptoms, which may manifest immediately or develop over time.
Clinical neuropsychological evaluation in TBI is crucial for understanding the full impact of the injury on a patient’s cognitive and behavioral functioning. This comprehensive assessment identifies the patient’s cognitive strengths and weaknesses, including areas such as memory, attention, problem-solving, language, and executive functioning. Neuropsychologists use different tools and techniques at various stages of recovery to monitor progress, adapt rehabilitation strategies, and predict outcomes. Early in the disorder, assessments may focus on basic cognitive functioning to guide immediate treatment and interventions. As the patient progresses, more detailed evaluations help refine the rehabilitation process, ensuring that it addresses evolving challenges like social skills, emotional regulation, and reintegration into daily life.
Neuropsychological testing also plays a critical role in differentiating between cognitive impairments caused by the brain injury itself and those resulting from emotional or psychological factors, such as depression or anxiety, which often co-occur in TBI cases. Moreover, these evaluations help inform decisions regarding the patient’s ability to return to work, school, or other activities, as well as the need for long-term support or accommodations.
The process of neuropsychological evaluation is typically multidisciplinary, involving collaboration with neurologists, physical therapists, speech-language pathologists, and occupational therapists. This integrated approach ensures that the patient’s care is comprehensive, addressing both the neurological damage and the broader impact on their quality of life.
Neurodegenerative diseases
Neurodegenerative diseases impact millions of people worldwide. These disorders involve the gradual loss of specific groups of neurons and disrupt important physiological processes such as proteo-toxic stress, oxidative stress, apoptosis, and neuro-inflammation, ultimately leading to progressive neuronal dysfunction and death. While some patients exhibit distinct symptoms, others may display a combination of clinical features.
Neurodegenerative diseases can be classified based on different criteria. They may be categorized according to primary clinical features, such as Alzheimer’s disease, Parkinson’s disease, and dementia. The anatomical distribution of neurodegeneration can also be used to classify these diseases, leading to categories like frontotemporal degenerations, extrapyramidal disorders, or spinocerebellar degenerations. Furthermore, the protein abnormalities observed in these disorders allow for further subcategorization into amyloidoses, tauopathies, α-synucleinopathies, and TDP-43 proteinopathies.
Neuropsychological measures help differentiate between normal cognitive aging and impairment that goes beyond typical aging. Baseline neuropsychological testing can determine whether an individual is experiencing normal age-related changes, providing valuable information for both the referring physician and the person being evaluated. This evaluation also offers an opportunity for neuropsychologists to support lifestyle factors that promote healthy aging while educating individuals about normal aging in the context of their unique cognitive strengths and weaknesses.
Neurocognitive disorders
Cognitive function significantly impacts an individual’s quality of life. As the population ages, the number of people developing neurocognitive disorders (NCD) is on the rise. The number of individuals with dementia is projected to double every 20 years and is expected to surpass 115 million worldwide by 2050. It is crucial to identify vulnerable individuals early, understand the progression of their NCD, and administer effective treatments.
Commonly diagnosed disorders include:
- Alzheimer’s disease (AD)
- Mild cognitive impairment (MCI)
- Parkinson’s disease (PD)
- Frontotemporal dementia (FTD)
- Lewy body disease (LBD)
- Progressive supranuclear palsy (PSP)
- Corticobasal degeneration (CBD)
- Wernicke-Korsakoff syndrome
Neuropsychological testing is a method used to evaluate neurocognitive disorders by relying on quantitative and clinical data to diagnose and describe the functioning of patients. This form of testing uses functional anatomic correlations to assess the functional integrity of underlying brain regions and processes. While it provides lateralization and localization information, the primary benefit of neuropsychological testing lies in quantifying cognitive skills and identifying subtle deficits early in the course of neurocognitive disorders. Additionally, it can distinguish between the contributions of neurologic and emotional functioning in patient symptoms and aid in directing treatment appropriately. This article outlines the process of neuropsychological testing in neurocognitive disorders and provides examples of the different skill deficits present in each disorder.
Brain-behavior relationships
The relationship between the brain and behavior can be seen as a modern version of the well-known mind-body dualism proposed by Descartes. In this view, the brain represents the physical or biological aspect, while behavior represents the mental or psychological aspect. Despite its historical roots, this mind-body duality remains an unresolved issue. These concepts have long been treated as separate and distinct, hindering scientific progress. In reality, the relationship between the mind and body is much more complex and intertwined.
Theoretical Foundations of Neuropsychology offer a framework for understanding how brain function and behavior are related, drawing on principles from both neuroscience and psychology. Neuroscience focuses on understanding how the nervous system influences behavior and applies this knowledge to guide clinical care for neurological and psychiatric disorders. One common approach to addressing this core question is to study brain-behavior associations across individuals, examining how variations in brain measures relate to variations in behavior.
Studying patients with brain damage provides an opportunity to explore the anatomy of brain functions, which has been enhanced by advancements in structural neuroimaging. Despite these advancements, uncertainties persist regarding the exact brain areas involved in specific processes. This contributes to ongoing controversies over the lesions associated with neuropsychological disorders. These uncertainties are largely due to the methods used in studying brain-behavior relationships, often relying on group comparison designs.
A comprehensive neuropsychological assessment examines brain-behavior relationships through tests that evaluate specific domains of brain functioning, particularly those sensitive to impairment resulting from brain damage.
Cognitive impairment diagnosis
Neuroanatomy and cognitive functions are closely related, as the structure of the brain directly influences various mental processes. Cognitive Impairment is defined as the “symptomatic pre-dementia stage” on the continuum of cognitive decline, characterized by objective impairment in cognition that is not severe enough to require help with usual activities of daily living. Cognitive decline and Cognitive Impairment have important implications for patients and their families and will require that primary care clinicians be skilled in identifying and managing this common disorder as the number of older adults increases in the coming decades. Current evidence supports aerobic exercise, mental activity, and cardiovascular risk factor control in patients with Cognitive Impairment.
Neuroanatomy of cognition is a complex and evolving field of study that explores the structural and functional bases of cognitive processes. Research in this area delves into the neural structures and pathways involved in cognitive domains, such as attention, memory, language, and decision-making.
A neuropsychological assessment involves the administration of standardized tests (with normative data) across a range of cognitive domains which typically include memory, language, visuospatial and perceptual functions, attention, and executive functions. The Montreal Cognitive Assessment is a quick and easy instrument that can be adapted for use in the clinical setting. It is easy to administer and score, and the results can be interpreted by the health provider with minimal training. Both an app and paper versions are available.
Clinical Neuropsychology and Technology
Historically, neuropsychological assessment has relied on paper and pencil-based tests to assess cognitive abilities, and studies conducted with these tests have generated thousands of scholarly articles promoting their strengths and debating their weaknesses. However, in recent years, increasing numbers of researchers and clinicians have started to use various technologies to improve the efficiency, reliability, and cost-effectiveness of neuropsychological assessment. Researchers are exploring Future Directions in Clinical Neuropsychology to enhance diagnostic methods and treatment approaches.
Rapid advances in technology, including improved computer programming, have allowed many assessment measures to be administered, scored, or interpreted without the direct interaction of a clinician. Advances in neuroimaging and neuropsychology have significantly enhanced our understanding of brain function and behavior, allowing researchers and clinicians to develop more effective interventions for various neurological and psychological disorders. Together, these advances are leading to improved diagnostic methods and therapeutic interventions. For instance, by correlating neuroimaging findings with neuropsychological assessments, practitioners can create more tailored rehabilitation programs for patients recovering from strokes or traumatic brain injuries. Additionally, the integration of artificial intelligence with neuroimaging data holds the potential to uncover hidden patterns, leading to early diagnosis of neurodegenerative diseases like Alzheimer’s.
Neuropsychological assessment
Neuropsychological assessment is the normatively informed application of performance-based assessments of various cognitive skills. Typically, neuropsychological assessment is performed with a battery approach, which involves tests of a variety of cognitive ability areas, with more than one test per ability area.
Neuropsychological tests are specialized tasks designed to measure psychological functions that are linked to specific brain structures or pathways. These tests are used both in research on brain function and in clinical settings for diagnosing deficits. They typically involve the systematic administration of clearly defined procedures in a formal environment. Neuropsychological tests are usually conducted with one person in a quiet office, free from distractions, while working with an examiner. Because of this controlled setting, these tests can sometimes provide an estimate of a person’s peak cognitive performance.
These tests are a core component of neuropsychological assessments, which also take into account personal, interpersonal, and contextual factors. Health provides clinicians with an objective and patient-friendly way to measure and monitor cognitive health.
Conclusion
Clinical neuropsychology is an essential field that connects psychology and neurology, focusing on how brain function influences behavior and cognitive processes. Its history showcases significant advancements in our understanding of brain-behavior relationships, evolving from early observations to sophisticated assessment tools and therapeutic interventions. This discipline plays a crucial role in enhancing our understanding of cognitive function and in guiding effective treatment strategies. As research continues to advance, clinical neuropsychology will likely refine its methodologies and expand its impact, promoting a more comprehensive approach to mental health and cognitive rehabilitation. Through ongoing interdisciplinary collaboration and technological advancements, clinical neuropsychology will remain at the forefront of addressing the complex relationship between brain function and psychological well-being.
Frequently Asked Questions
Frequently Asked Questions about clinical neuropsychology:
What is the difference between clinical psychology and clinical neuropsychology?
the main difference between psychology and neuropsychology is in their approaches to how they address psychological conditions. Psychologists focus more on emotions, while neuropsychologists focus on neurobehavioral disorders, cognitive processes, and brain disorders.
What is the difference between psychiatry and clinical neuropsychology?
Perhaps the biggest difference between psychiatry and clinical psychology is that all psychiatrists go to medical school and become MDs, while psychologists don’t. Because of this, psychiatrists are able to prescribe pharmaceuticals, while most psychologists can’t.
What is the difference between clinical and applied neuropsychology?
Clinical psychology assesses and treats mental, behavioral and emotional problems, whereas applied psychology applies psychological science and theories to address real-world issues.
Can a clinical neuropsychologist diagnose ADHD?
Neuropsychologists are specifically trained in brain functioning, neuroanatomy, and brain-behavior relationships. Therefore, when assessing for ADHD, a neuropsychologist may use a variety of standardized cognitive tests and behavioral questionnaires.
References:
https://pubmed.ncbi.nlm.nih.gov/29936902
https://pubmed.ncbi.nlm.nih.gov/27090578
https://pubmed.ncbi.nlm.nih.gov/27684307
https://pubmed.ncbi.nlm.nih.gov/27685094
https://pubmed.ncbi.nlm.nih.gov/32964786
https://pubmed.ncbi.nlm.nih.gov/34791971
https://pubmed.ncbi.nlm.nih.gov/38914558
https://pubmed.ncbi.nlm.nih.gov/30513257
https://pubmed.ncbi.nlm.nih.gov/33138689
https://pubmed.ncbi.nlm.nih.gov/35658794
https://pubmed.ncbi.nlm.nih.gov/30020682
https://pubmed.ncbi.nlm.nih.gov/31334941
https://pubmed.ncbi.nlm.nih.gov/38763778
https://pubmed.ncbi.nlm.nih.gov/37073481
https://pubmed.ncbi.nlm.nih.gov/29214891
https://pubmed.ncbi.nlm.nih.gov/29923448




